Diagnosis of respiratory diseases through lung sounds remains one of the most complex clinical tasks. Even experienced physicians admit that auscultation results are often subjective: one specialist hears a pathology, while another does not. Yet these judgments influence critical decisions – whether to hospitalize a patient, prescribe antibiotics, or assess the severity of their condition.
This uncertainty is especially evident in primary care – in outpatient clinics, nursing homes, and during TeleMedicine consultations. When a physician cannot involve a pulmonologist, the cost of error increases. Machine learning and sound analysis technologies are paving the way toward a more objective assessment of respiratory sounds and earlier detection of lung diseases.
In recent years, a wave of medical devices has emerged that aim to help clinicians not only hear or see but also interpret the body’s signals through data. From retinal image analysis algorithms to ECG monitors trained on millions of recordings, intelligent auscultation is a natural extension of this trend.
We are speaking with Helena Binetskaya – Co-Founder and Chief Product Officer of the company – about this shift, and about her team’s solution, ChestPal® Pro, which combines the classical method of listening with artificial intelligence.

2digital: How would you explain ChestPal in simple terms to someone outside the medical field? What does the device actually do, and what can a user see within the first 60 seconds?
Helena: ChestPal Pro is a smart stethoscope that automatically classifies lung sounds to help healthcare providers diagnose and monitor respiratory conditions.
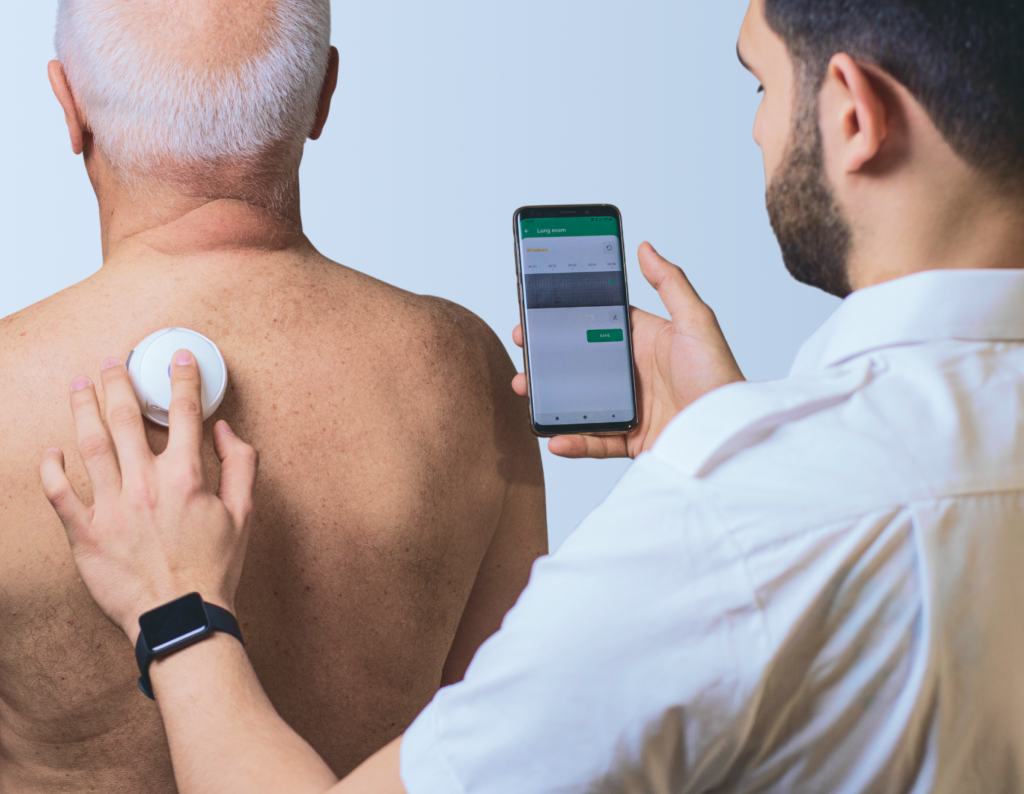
Lung sounds can be faint and difficult to detect with confidence. ChestPal Pro reliably detects and categorizes sounds into normal and abnormal lung sounds. At the click of a button, it connects to our smartphone app and, when the device is placed on the chest, a second click of that button initiates a 5-second recording of the lungs. This recording is analyzed, and the result is instantaneously displayed on the app. The results are presented visually and audibly. They can be saved or replayed to aid assessments over time and are easily shared with medical professionals over email or messenger apps.
2digital: What makes ChestPal fundamentally different from a traditional or even a “digital” stethoscope? Where does the real innovation lie: in the hardware, the DSP/AI layer, or the data?
Helena: It takes the traditional stethoscope – which has not changed substantially since its inception in 1816 – and flips it on its head. The limitations of traditional stethoscopes include lack of amplification, low clarity, no recording capability, no sound classification, and no sharing of results. Their performance is entirely user-dependent, with subjectivity leading to high inter- and intra-rater variability, thus reducing its clinical utility.
Digital stethoscopes provide sound amplification and a recording that can be shared, but no analysis or sound classification is provided, and the interpretation of recorded sounds remains entirely subjective.
Rather than simply amplifying lung sounds, ChestPal deploys a patent-protected neural network algorithm that was trained using a proprietary dataset of lung sounds labelled by a panel of expert pulmonologists. It provides not only amplification, clarity, recording, and sharing but also classification of the lung sounds together with a visual time/frequency spectrogram. The results provided by ChestPal aid diagnosis and monitoring, timely patient treatment, and ultimately better outcomes for patients. This also helps bridge care gaps where access to specialists is restricted – for example care homes or rural areas.
2digital: What kind of validation or clinical studies support ChestPal’s accuracy? Are there any independent trials or peer-reviewed publications comparing your system to expert auscultation or standard diagnostic methods?
Helena: ChestPal’s accuracy and reliability is supported by peer-reviewed clinical studies presented in the European Respiratory Journal.
“The abstract, automatic lung sound analysis accuracy: a validation study” was presented at the 2021 European Respiratory Society International Congress, in the session “Prediction of exacerbations in patients with COPD”, (N=110 adults). The demonstrated overall accuracy of the device in classifying lung sounds was 81.6%. In comparison, published clinical evidence suggests the frontline healthcare providers detect lung sounds with a sensitivity of 61–65%.
Further evidence comes from “Automated lung sound analysis using the ChestPal Pro platform: a sensitive and specific tool for identifying lower respiratory tract involvement in COVID-19.” A prospective observational study with 314 participants demonstrated sensitivity of 94.0% and specificity of 96.9% at identifying lower respiratory tract involvement, defined as presence of abnormal lung sounds in two or more auscultation points. Diagnostic imaging was a gold standard to confirm diagnosis.
2digital: How does ChestPal perform in noisy environments or when the sensor is placed incorrectly? How do you handle artifacts, breathing patterns, or patient variability?
Helena: ChestPal was trained to recognise artifacts including external noise, such as talking, and patient variability across age groups, pathologies, etc., which is integral to the data set used to train the ANN.
As with all stethoscopes, the correct auscultation protocol should be followed: auscultate in a quiet environment, have the patient breathe quietly though an open mouth, and hold the stethoscope still on the skin.
2digital: How often do clinicians actually use the visual data displayed by your device, rather than relying on AI tags alone? Do you plan to build educational tools to help interpret these visuals?
Helena: Spectrograms offer a visual representation of the various frequencies in a waveform over time, along with the strength or amplitude of each frequency. The spectrogram created in the ChestPal app may help healthcare professionals see subtle sounds that are hard to hear and be used as a training aid. This is supported by an article in Nature, which states, “Thus, we conclude that the use of spectrograms had a positive impact on the inter-rater agreement and the agreement with experts. We observed a higher improvement in the classification of crackles compared to wheezes.”
We provide user training and have a suite of educational tools to support clinicians with auscultation in general, including typical lung sounds and their spectrograms.

2digital: What is the current regulatory status of the device and software in the US and EU? After the US launch announcement, what are the next milestones toward full certification and compliance?
Helena: ChestPal is registered with the FDA and actively marketed in the US, and CE (MDR) is in the company’s regulatory pipeline.
2digital: How do you ensure secure data sharing between clinicians: HIPAA, GDPR, or other regional standards?
Helena: The system is HIPAA and GDPR-compliant, with the transfer of only anonymized patient data.
2digital: In practice, what tends to be the hardest part of scaling or piloting ChestPal: clinician training, workflow integration, procurement, connectivity, or trust?
Helena: Typical of any new advancement in medical technology, user training is the biggest challenge, especially when clinicians struggle to break old habits developed over many years of traditional stethoscope use. ChestPal provides an extensive in-app onboarding module and in-person in-service training.
2digital: Looking 3–5 years ahead, how do you see the role of “smart auscultation” evolving in primary care and TeleMedicine? Will it become a triage tool for every nurse, a home device for chronic patients, or simply an extra “pair of digital ears” for doctors?
Helena: Yes – all of the above, and far more than an extra pair of ears for doctors!


