AI remote patient monitoring seeks to address a longstanding and complex challenge in medicine: translating chaotic streams of health data into a comprehensible and standardized format. This capability empowers medical professionals to prioritize effectively and respond to challenges in a timely manner. The primary “superpower” of AI is transforming a thousand signals, ex. heart rate spikes, into a single, actionable notification: “Pay attention, there is a problem!”
Today, we will discuss what RPM is, where AI fits into remote patient monitoring, what the evidence base says, which trends are noticeable, and how to avoid turning a project into an expensive factory of useless notifications.
What is Remote Patient Monitoring and Remote Patient Monitoring Technology?
Remote patient monitoring (RPM) is the collection of a patient’s physiological data outside the clinic (at home) using connected devices and its transmission to a system where this data can be reviewed and utilized by healthcare workers for patient management.
RPM is not just a “gadget,” but a whole care delivery model where data on a patient’s condition is collected outside the clinic and regularly used by a healthcare team to manage the patient.
It is worth distinguishing RPM from “self-control”: if a person measures their blood pressure for themselves, that is self-tracking. If the data goes into a system and there is a protocol for the medical team’s reaction, that is RPM (in the sense of the CMS approach).
What are RPM Devices?
The Centers for Medicare & Medicaid Services (CMS) cite devices that collect metrics such as blood pressure, weight, and glucose and transmit this data to healthcare providers as examples.
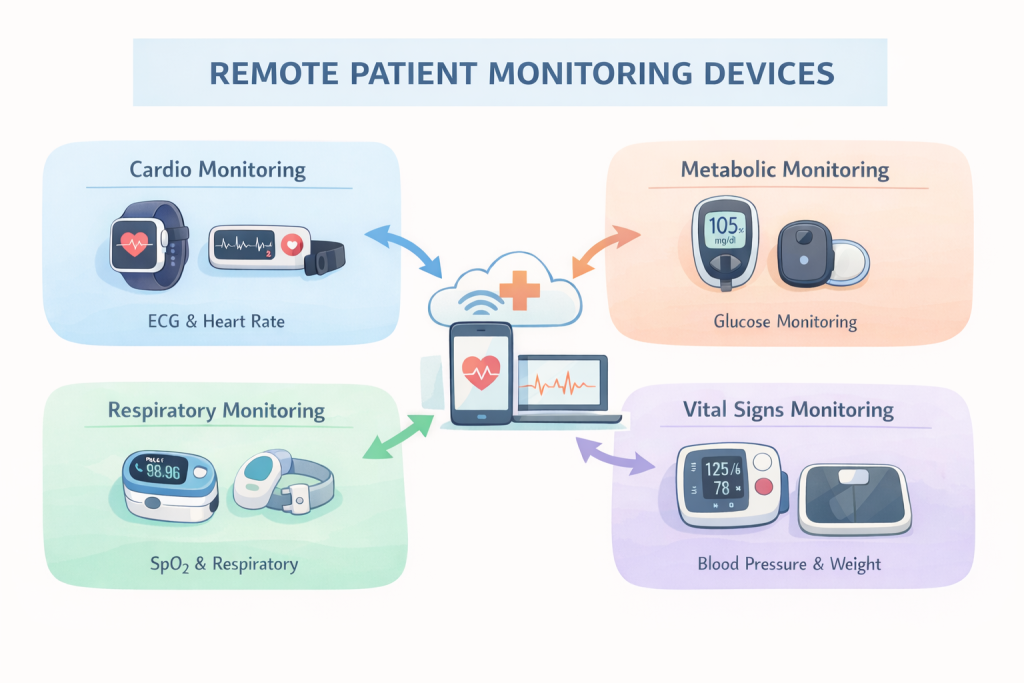
Primary RPM devices are categorized by several criteria:
By signal type – what they measure:
Cardio: Pulse/heart rate, sometimes ECG (wearables, patches, standalone monitors).
Respiration: SpO₂ (pulse oximeters), sometimes respiratory rate.
Metabolism: Glucose (glucometers/CGM), weight.
Vitals: Blood pressure (blood pressure monitors/cuffs).
By “clinical seriousness”:
Consumer/wellness devices: Fitness trackers and similar gadgets—useful for observation but not always designed for clinical decision-making.
Medical-grade devices: Tools created specifically for medical use, typically adhering to stricter standards regarding accuracy and documentation.
By data transmission method:
Automatic transmission: Data is sent without human intervention.
Semi-automatic/manual: The patient enters the data themselves.
We have collected the information, what comes next?
The primary advantage gained through AI is the speed and quality of data processing.
Without AI, remote patient monitoring risks devolving into a beautiful yet meaningless stream of numbers. Let us examine two critical processes: data normalization and analytics.
The primary objective of normalization is to transform disparate measurements into standardized clinical data. In RPM, data arrives in varying types, qualities, and formats. If all of this is simply dumped into a single folder, the physician is left with chaos. Consequently, normalization is essential — transforming “raw material” into a uniform, comparable stream of patient data.
What normalization typically includes:
Standardization: Adopting uniform formats and units of measurement, ensuring data is attributed to the correct individual and context.
Time Alignment: One device measures daily, another every five minutes; the platform must reconcile everything into a coherent timeline.
Cleaning: Removal of duplicates and “noise”.
Interoperability: Data must be able to “live” within clinical systems, remaining intelligible to electronic health records and clinical platforms. For this, standards such as HL7 FHIR are employed.
Once normalization is complete, the foundation is laid for the most valuable asset: AI in remote patient monitoring services transforms the stream of numbers into a clear picture and an actionable list—identifying what can be ignored, what warrants verification, and where urgent intervention is required. This is not “diagnosis,” but rather an effort to ensure the clinician sees what matters most.

Here are the key tasks of analytics in AI-driven remote patient monitoring:
Data Cleaning and Quality Control (Data Quality). Even normalized data can be flawed: motion artifacts, poorly positioned sensors, gaps, and malfunctions. AI can identify suspicious segments, reduce the impact of “noise” on the overall picture, and flag data that cannot be trusted. Without this, the clinic drowns in alerts and manual verification.
Anomaly Detection. A threshold like “heart rate over 100” is a blunt instrument. AI approaches this differently: it looks for deviations from a specific individual’s established norm, analyzing dynamics and signal combinations. This is useful for “noticing oddities” early, before a dangerous situation becomes obvious.
Risk Forecasting (Prediction). The next level is an attempt not just to evaluate “oddities,” but to hypothesize their consequences. On time series data, AI models can search for patterns of deterioration and highlight patients at increased risk (depending on the clinical scenario and available data).
Triage and Notification Prioritization. This is the most “applied” effect of remote patient monitoring with AI — a doctor or nurse sees not “500 events in the stream,” but, hypothetically, “5 specific patients to contact today”. It is in this part that one of the main pain points of RPM is addressed: the burden on staff, who tire of the multitude of daily notifications and lose control over them. This combats the phenomenon of “alert fatigue” — a situation where the system screams “urgent!” too often, and the specialist eventually stops responding to such messages with the necessary attention.
The Evidence Base: Tangible Improvements from RPM and the Role of AI
One cannot claim that AI-enabled remote patient monitoring is a flawlessly perfected process. Much depends on the specific field of application: in some areas, results are more successful, while in others, they are less so. Here are the trends that can be identified.
Fewer admissions and hospitalizations — often, but not always. A systematic review of RCT studies on device-based remote monitoring notes that a decrease in hospital service use was observed in the majority (72%) of the included trials.
A 2024 review also explores “sensor-based alert systems,” noting an average 9.6% reduction in hospitalizations and a 3% average reduction in all-cause mortality.
Frequently applied in heart failure and cardiac monitoring. There are large-scale studies on the impact of remote monitoring in heart failure (including hospitalization rates and quality of life). The conclusions note that if a person has heart failure, RPM generally helps them avoid hospitalization specifically due to this disease. Regarding whether it helps extend life, the effect appears possible, but authors do not consider the evidence sufficiently robust. At the same time, according to researchers, in real life, the result depends not only on the device but also on how quickly and precisely the medical team reacts to signals.

COPD/Respiratory Diseases: Effects Depend on the Model. A systematic review conducted in 2022 showed that, on average across the market and studies, the evidence is weak and the effects are inconsistent. In particular, it was noted that, on average, remote home monitoring (RHM) did not demonstrate a stable improvement in quality of life, lung function, or “confidence in disease management,” nor did it yield a sustained reduction in visits/hospitalizations. However, it was noted that when monitoring was accompanied by regular feedback from medical professionals, COPD-related hospitalizations could decrease.
A research from 2025, studying the pilot implementation of home telemonitoring for patients with chronic obstructive pulmonary disease in the public healthcare system of Andalusia (Spain), showed more optimistic results: exacerbations decreased by 44.3%, hospitalizations by 51.58%, and patients noted an improvement in quality of life. But it is important to understand that since this is not an RCT and there is no control group, the result could be strongly influenced by the specifics of this particular implemented system. In other places and under other conditions, the effect might be quite different.
Diabetes and remote patient monitoring. Another publication describes the effect of remote glucose monitoring in the context of diabetes management. It discusses a program where the clinic constantly viewed the patient’s glucose data, and patient-doctor contact occurred every 2–3 weeks. The medical professional received recommendations formed on the basis of remote monitoring and computer algorithms for insulin dose correction.
Diabetes control among program participants improved noticeably. For the majority of patients, an insulin dose increase of approximately 30% was required. For a substantial portion of patients (36%), insulin doses did not increase (or even decreased), yet diabetes control still improved.
Trends: The Direction of Remote Patient Monitoring AI
More passive sensors and continuous monitoring. Remote monitoring is gradually moving away from the “patient remembers – measures – sends” model to one where data is collected almost without human participation. For the patient, this feels like a relief: fewer routine actions and fewer chances to “forget to measure.” For the clinic, it offers a potentially more accurate picture and complete dynamics. When talking to a patient, a doctor will see that a metric is not just bad today but has been trending negatively for a week.
However, this trend has a downside: continuous monitoring means an avalanche of data. The more measurements, the more noise, artifacts, and random spikes. Therefore, passive sensors almost automatically necessitate intelligent processing: filtering, signal quality assessment, normalization, and triage.

Governance and trust are becoming “part of the product.”
Until recently, many AI products in healthcare sold themselves with a single phrase: “we have high accuracy.” Now, this is increasingly insufficient. Governance involves answers to boring but vital questions: who is responsible for the model; how quality is verified; what happens if the algorithm starts making mistakes; how decisions and alerts are recorded; and how the model is updated without disrupting the clinical process.
Gartner analysts, in their list of strategic trends for 2025, specifically highlighted themes related to the trustworthy implementation of technologies.
In practice, this will look grounded: products will have clear “boundaries of applicability,” logging (why an alert was triggered), a transparent update policy, and quality monitoring in production. Otherwise, clinics and regulators will treat AI in monitoring as a potential source of risk, even if the idea itself is good.
Legislation Influences Roadmaps. This trend is the most unpleasant for those who prefer the “let’s build an MVP first and deal with the rules later” approach. In Europe, the EU AI Act is already a law with legal force and a phased introduction of requirements. This means that product roadmaps are beginning to depend on when and which specific requirements become mandatory.
This is important for AI in RPM because medical scenarios and systems that impact health very often fall into zones of heightened scrutiny: they require greater transparency, risk management, documentation, and quality control.
Ultimately, the winners are those who perceive regulation not as a brake, but as a component of product engineering: building processes, documentation, quality monitoring, and change management in advance. For the market, this also serves as a filter: some players will be eliminated not due to technology, but due to a lack of implementation discipline.


