Healthcare AI has attracted record investment and hype: by 2024, 78% of organizations reported using AI somewhere in their operations. What’s less clear is how much these deployments improve efficiency and productivity. Donald M. Berwick and colleagues estimated that in U.S. healthcare, about 30% of spending delivers little benefit, so algorithms alone won’t solve the problem. In this article, we are trying to find an answer: is AI in healthcare actually delivering efficiency gains, or are we seeing a productivity paradox – rapid tool adoption without a measurable payoff?
Are there measurable productivity gains?
In economics, Total Factor Productivity (TFP) measures the output not explained by labor and capital inputs – essentially the efficiency boost from innovation. If AI were dramatically improving healthcare efficiency, we would expect to see it in TFP or related productivity metrics. So far, however, it’s challenging to find clear evidence of AI-driven productivity gains in healthcare. Health output is hard to quantify – better patient outcomes don’t neatly translate into “productivity” in monetary terms, and any improvements may be swamped by rising costs or increased service complexity.
Historically, general purpose technologies have lagged in showing up as productivity gains. In fact, new technologies often require complementary changes – processes, skills, and infrastructure – before their potential is realized.
Another issue is output mismeasurement. AI might improve the quality of care, e.g. more accurate diagnoses, fewer adverse events without immediately reducing costs or staffing needs. Traditional productivity metrics might not capture these quality improvements. For instance, if an AI detects more early-stage cancers, the health system does more procedures – raising costs now, but saving lives and future costs. In pure productivity terms, it could look like more input for the same output. Such nuances make it tricky to ascertain AI’s contribution from top-line numbers alone.
The Stanford AI Index 2025 report notes a growing body of research confirming AI can boost productivity in various industries, but it’s not straightforward to calculate a “TFP of healthcare AI” at this stage. It may simply be too early – AI adoption in healthcare is nascent, and as with past innovations, efficiency gains might only emerge after a significant lag.
Historical trends: AI’s potential speed from innovation to productivity
Major technological innovations in the past took decades to yield economy-wide productivity gains. The steam engine, pioneered in the 1700s, took roughly 61 years before its benefits showed up in productivity statistics; electricity needed about 32 years; and the Internet needed about 15 years. AI is still in its early days – its full impact on productivity is to be determined, but many believe the lag will be shorter, potentially under a decade, if historical trends hold.
The bar chart above underscores a hopeful trend: each successive general-purpose technology has reached productivity payoffs faster than the last.
Jamie Dimon, CEO of JPMorgan, notes that if the historical trend of shortening lags holds, AI’s productivity boost could appear in economic data by the late 2020s. Optimistically, AI might deliver a productivity bump in as little as seven years – half the time it took PCs to make a dent. This is fueled by the breakneck speed of AI advancement and adoption. For example, generative AI tools (ChatGPT and the like) reached 100 million users within months, suggesting a faster diffusion than any prior tech.
However, the mere presence of a revolutionary technology does not guarantee immediate productivity gains. The famous case of electric motors illustrates why. In the late 19th century, factories that swapped steam engines for electric motors initially saw little improvement – managers simply bolted the new motors into old layouts, missing the real opportunity. Only when factories reconfigured, moving from one giant motor driving all machines via belts to individual motors on each machine (the “unit drive” system) did productivity surge.
Big promises: $200–$360 billion in projected savings If AI’s impact is hard to see now, proponents argue it’s coming soon – and will be huge. A comprehensive 2023 study by Harvard and McKinsey researchers estimated that wider AI adoption could save 5–10% of U.S. healthcare spending, roughly $200–$360 billion annually.
Notably, they based these figures on current AI technologies and achievable use cases within approximately five years, assuming quality of care isn’t compromised. Where would such massive savings come from? The study breaks it down by stakeholder, highlighting different areas of efficiency gains:
Hospitals – Optimizing clinical operations, enhancing quality and safety. Potential savings: 4–11% of hospital costs (~$60–$120 billion per year);
Physician groups – Streamlining administrative and care continuity tasks. Projected savings: 3–8% of practice costs (~$20–$60 billion annually);
Payers (health insurers) – Improving claims processing and better managing care to avoid costly complications. Estimated impact: 7–9% of insurer costs (~$80–$110 billion per year).
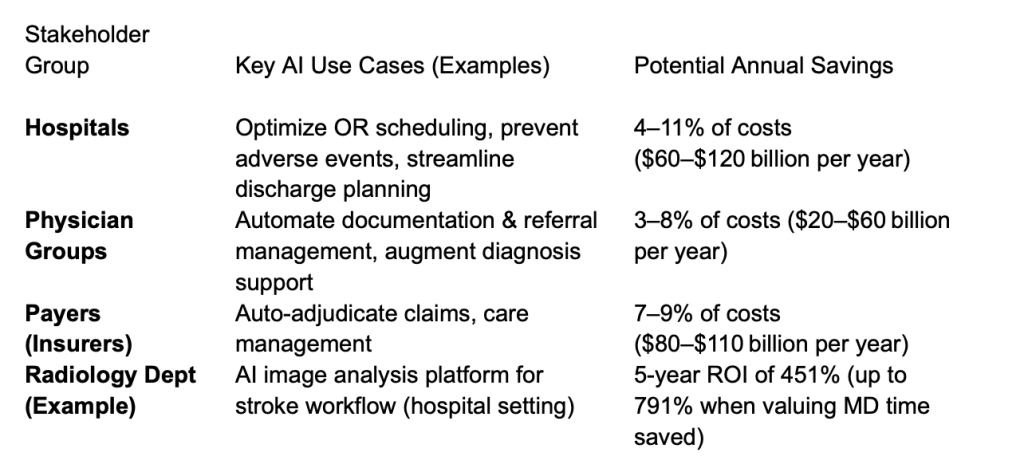
A separate study in radiology demonstrates how, in a specific clinical domain, an AI tool can yield a very high return on investment (ROI) by saving clinician time and improving throughput. These projections assume effective implementation of currently available AI use cases within approximately five years.
But are these savings materializing in practice? So far, the evidence is thin. The report itself acknowledges that healthcare has lagged behind other industries in AI adoption – meaning much of this opportunity is still untapped. It’s essentially a potential savings estimate, predicated on overcoming adoption barriers. Real-world data is needed to validate that these efficiencies can be achieved outside of models and pilot programs.
Early ROI evidence: radiology as a test case
One area where AI is relatively mature is medical imaging (radiology). Imaging AI was among the first wave of FDA-cleared tools, and radiologists have been experimenting with AI for tasks like detecting lung nodules or prioritizing critical scans. A recent study in the Journal of the American College of Radiology attempted to quantify the ROI of a comprehensive AI platform in a hospital radiology department. The results were striking: over a 5-year period, implementing the AI system yielded a 451% ROI, which jumped to 791% when factoring in the monetary value of radiologists’ time saved. In concrete terms, the AI saved radiologists in the order of 145 working days over five years.
This sounds like a resounding success – who wouldn’t invest $1 to get $4.50 (or $8) back? However, caution is warranted before generalizing these results across the entire healthcare system. Radiology is somewhat unique – it’s technology-intensive, highly digital, and throughput-oriented. An AI that shaves minutes off per scan reading or flags urgent cases faster can directly translate into more studies read per day and better patient outcomes, e.g. faster stroke interventions. Not all of healthcare has this dynamic. In many clinical areas, if AI saves a doctor 15 minutes, it may simply mean they spend that time with another patient, improving care quality or volume, which is great, but it doesn’t necessarily reduce costs unless the practice structure changes.
Moreover, the ROI calculator in the study made certain assumptions – e.g. a hospital has a stroke center accreditation, a high baseline scan volume, and the ability to capitalize on newly identified findings. If those assumptions change to, say, a small community hospital with lower volumes, the ROI would likely be more modest. The study’s authors themselves note that results were sensitive to factors like the time period and number of scans performed.
AI’s financial payoff in healthcare might be highly context-dependent.
Obstacles or why AI hasn’t transformed healthcare (yet)
If the potential is so great, what’s preventing measurable efficiency gains? Healthcare faces several entrenched obstacles that create a lag between technological innovation and tangible performance improvement:
Data quality and integration;
Trust, adoption, and workflow alignment;
Misaligned incentives and ROI uncertainty;
Regulation and liability;
Infrastructure and training needs.
The slow pace of demonstrated productivity gains from AI in healthcare isn’t due to the technology failing – it’s more about the context in which it’s deployed. Data problems, cautious culture, misaligned incentives, and the complexity of healthcare delivery all act as friction. The technology is ready, but the system is not, at least not uniformly so. This is the essence of the productivity paradox in healthcare, where you have advanced AI tools available, yet the day-to-day operations in many clinics and hospitals look no more efficient than before. Bridging that gap requires as much work in people, process, and policy as in technology.
Paradox or just patience?
So, are we facing a performance paradox? At present, yes – it appears we have not yet seen the productivity surge that AI promises, despite the proliferation of tools. But this paradox may resolve itself with a little more time and targeted effort. It’s possible that we’re on the cusp of the upswing of what economists like Erik Brynjolfsson call the “J-curve,” where productivity initially dips or stays flat as organizations invest in intangibles (training, process redesign), then climbs sharply once the new system clicks. We might simply be in the transition period where AI is being integrated and aligned with healthcare workflows. If that’s the case, patience is warranted before passing judgment. The next few years will be telling; by 2028 or 2030, if AI truly is the general-purpose technology it’s touted to be, we should start to see clearer signs of faster service, lower admin overhead, and maybe even bending of the cost curve in some areas of healthcare.
Conversely, what if the productivity boost never fully materializes? That scenario would force reflection on whether AI is delivering primarily quality improvements (better medicine but not cheaper medicine) or whether systemic issues in healthcare like misaligned incentives are so strong that they can absorb even a powerful technology’s potential efficiency gains.


